Stages of Alcoholism
Stages of Alcoholism
Alcoholism was identified in 1956 as an illness by the American Medical Association (AMA). It's a disease
—an altering of the brain that controls a person's motivation and ability to make healthy choices.
Once it takes hold, it can be hard to shake loose—without the right help.
There are factors that pop up again and again when determining who might have an issue with alcoholism. The first factor is the age at which a person has his or her first drink (the younger people are when they first start drinking, the more likely they are to drink more heavily into adulthood); the other factors are genetics and environment. If you're in the "at-risk" population, it doesn't take much to become dependent on alcohol or other drugs. No one plans on becoming dependent.
The most destructive form of alcoholism is chronic alcoholism, an emotionally, socially and physically devastating disease. Alcoholism emerges from alcohol abuse, when there's a pattern of drinking despite negative consequences. Alcoholism and alcohol abuse are both categorized as alcohol use disorders—affecting people of all ages and stages of life. The severity of the disorder lies on a spectrum, ranging from mild to severe dependence, also known as chronic alcoholism (although even a mild disorder can spiral out of control without early treatment). Many people can drink alcohol and not become addicted. But for some, drinking alcohol leads to alcoholism.
The Stages of Alcoholism: Recognizing the Signs
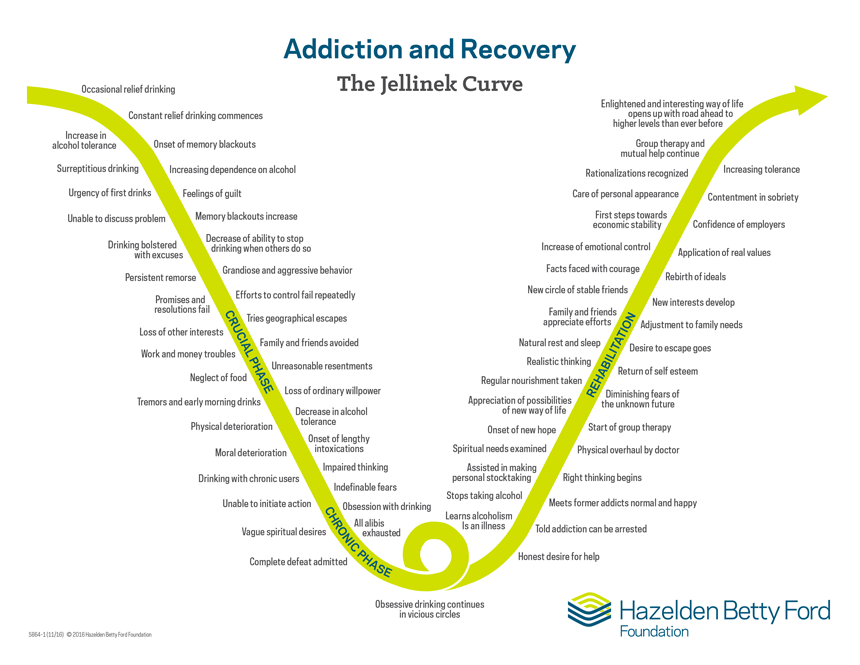
The Jellinek Curve, created by E. Morton Jellinek in the 1950s and later revised by British psychiatrist Max Glatt, is a chart that describes the typical phases of alcoholism and recovery. The point of this research was to show that alcohol addiction is a progression and there's a "vicious circle" associated with obsessive drinking, with much to lose along the way if people don't seek help. The curve shows that life can get worse if the cycle of dependence isn't broken, but it can also get better through recovery.
Stage 1: Pre-Alcoholic
Do you drink to feel better about yourself? Do you drink to dull the pain? Do you drink to forget, stop worrying, or eliminate anxiety? If so, your drinking could escalate without help.
Stage 2: Early Alcoholic
Blacking out from drinking too much is a warning sign of this stage, along with lying about drinking, drinking excessively, and thinking obsessively about drinking.
Stage 3: Middle Alcoholic
At this point, it's obvious to those close to you that you're struggling. You might miss work, forget to pick up the kids, become irritable, and notice physical signs of alcohol abuse (facial redness, weight gain or loss, sluggishness, stomach bloating). Support groups can be a highly effective form of help at this stage.
Stage 4: Late Alcoholic
At this stage, drinking becomes everything in your life, even at the expense of your livelihood, your health and your relationships. Attempts to stop drinking can result in tremors or hallucinations, but therapy, detox, and rehab can help you get your life back.
Stage 5: Recovery
Once stabilized, the goal is to transition from detox, to treatment, to maintenance (practicing sober living by changing your life), to transcendence—the final step in the path to recovery.
The Jellinek Curve is a chart that describes the typical phases of addiction and recovery:
Do You Need Help? 10 Warning Signs of Alcoholism
Recognizing the symptoms of alcoholism can make a tremendous difference in getting proper treatment and heading down the path to recovery. Some warning signs include:
-Drinking more than planned or intended
-Failing to fulfill obligations at school, work or home (making drinking a priority, despite responsibilities, leading to missed school or work)
-Continuing to use despite negative impacts on relationships, financial situation or health
-Using in situations that could be physically hazardous, like drinking and driving
-Showing an increased tolerance to alcohol (drinking more in order to achieve the same desired effect). Because the brain changes with alcohol abuse, one of the first physiological signs of addiction is building up a tolerance.
-Experiencing physical or psychological withdrawal symptoms when attempting to stop drinking (anxiety, depression, insomnia, nausea, sweating, hand tremors/"the shakes," confusion, seizures and visual hallucinations)
-Losing interest in once-enjoyed activities or becoming socially isolated
-Becoming dishonest or secretive, aggressive, moody, or temperamental—people who have an alcohol addiction will try to hide it.
-Craving alcohol, such as drinking first thing in the morning
-Spending an inordinate amount of time thinking about drinking, acquiring alcohol, and recovering from hangovers
Some Physical Signs and Symptoms of Alcohol Addiction
-Rapid weight gain or loss
-Slow or staggering walk
-Inability to sleep or stay awake
-Unexplained bruises or marks
-Glazed or red eyes
-Cold, sweaty palms or shaking hands
-Puffy face, blushing or paleness
-Nausea, vomiting or excessive sweating
-Low or no energy
-Depressed or anxious
-Deterioration of personal appearance or hygiene
If you think a family member or loved one might be showing signs, signals or symptoms of alcoholism, know that it won't "go away" on its own. Their brain is changing—and without help, there can be serious long-term consequences. According to the National Institute on Alcohol Abuse and Alcoholism, "an estimated 88,000 people die from alcohol-related causes annually, making alcohol the third leading preventable cause of death in the United States." Learn more about alcohol addiction and treatment.
Long-Term Health Problems Associated with Chronic Heavy Drinking
Alcohol travels from the stomach and intestines through the bloodstream, overloading the liver's ability to process alcohol, directly affecting the brain's neurons, potentially converting alcohol into carcinogens, and taking its toll on the heart, pancreas, nervous system, joints and immune system. Heavy alcohol consumption has been linked to more than 60 different diseases.
Cancer
Based on extensive reviews of research studies, there is strong scientific consensus of an association between alcohol consumption and several types of cancer. In its Report on Carcinogens, the National Toxicology Program of the US Department of Health and Human Services lists alcoholic beverages as a known human carcinogen. The research evidence indicates that the more alcohol a person drinks—particularly the more alcohol a person drinks regularly over time—the higher his or her risk of developing an alcohol-associated cancer. Scientists believe that alcohol is converted into acetaldehyde, a potential carcinogen. Cancer of the mouth, throat, esophagus, liver, colorectal region, and breast have all been linked to heavy alcohol use.
The Million Women Study in the United Kingdom (which included more than 28,000 women with breast cancer) provided a recent estimate of breast cancer risk at low to moderate levels of alcohol consumption: every 10 grams of alcohol consumed per day was associated with a 12 percent increase in the risk of breast cancer.
Brain damage
According to the National Institute on Alcohol Abuse and Alcoholism, even mild alcohol use can affect the brain by:
Creating difficulty walking
Blurring vision
Slurring speech
Slowing reaction times
Impairing memory
The long-term impact on the brain depends on a number of factors, including:
How much and how often a person drinks
The age at which he or she first began drinking and how long he or she has been drinking
The person's age, level of education, gender, genetic background and family history of alcohol abuse
Whether he or she is at risk as a result of prenatal alcohol exposure
His or her general health status
The affects can range from dementia and intellectual functioning to debilitating conditions that require long-term care, even if a person has been sober for a period of time.
Cardiovascular disease
Binge drinking can lead to blood clots, which can lead to heart attacks, stroke, cardiomyopathy (a potentially deadly condition where the heart muscle weakens and fails) and heart rhythm abnormalities.
Cirrhosis of the liver
Our liver filters out harmful substances, cleans our blood, stores energy and aids in digestion. Too much alcohol can be toxic to liver cells, causing dehydration and permanent scarring—which ultimately affects the blood flow. Cirrhosis of the liver, according to the Mayo Clinic, is "late stage scarring caused by liver diseases and conditions, such as hepatitis and chronic alcoholism." Basically, alcohol damages the organ, and it tries to repair itself by forming scar tissue. With excessive alcohol consumption, this important organ can't metabolize Vitamin D, which could develop into a deficiency. Some common signs and symptoms of cirrhosis include fatigue, itchy skin, weight loss, nausea, yellow eyes and skin, abdominal pain and swelling or bruising. Advanced cirrhosis can be life-threatening.
Pancreatitis
Alcohol causes the pancreas to produce toxic substances that can eventually lead to pancreatitis, a dangerous inflammation and swelling of the blood vessels in the pancreas that prevents proper digestion. Severe abdominal pain and persistent diarrhea, as a result, is not fixable.
Immune system
Drinking too much can weaken your immune system, making your body a much easier target for disease. Chronic drinkers are more liable to contract diseases like pneumonia and tuberculosis than moderate drinkers. Drinking a lot on a single occasion slows your body's ability to ward off infections–even up to 24 hours after getting drunk.
Symptoms of Alcohol Detox
With so many effects on the body, the usual first step in treating alcoholism is detox—or getting alcohol out of your system. Depending on the severity of the alcohol use disorder, this stage can be mildly annoying or severe. Early withdrawal symptoms include headaches, anxiety, nausea, irritability and shaking.
Other withdrawal symptoms may include:
Chills
Alcohol cravings
Muscle cramps
Irritability
Palpitations (rapid heart rate)
Disorientation
Tachycardia (rapid heart rate)
Hypertension
Low-grade fever
Mood changes
Slurred speech
Impaired gait
Poor dexterity (skill with hands)
Fatigue
Abdominal pain
Loss of appetite
Additional symptoms can be seen several hours to a few days after stopping alcohol use and may include:
Autonomic hyperactivity
Increased hand tremor
Insomnia
Nausea or vomiting
Transient hallucinations or illusions
Psychomotor agitation
Anxiety
Grand mal seizures
The most severe form of alcohol withdrawal is delirium tremens (DTs), characterized by altered mental status and severe autonomic hyperactivity that may lead to cardiovascular collapse. Only about 5 percent of patients with alcohol withdrawal progress to DTs, but about 5 percent of these patients die.
Because of its high mortality, DTs is a medical emergency. Signs and symptoms, which may worsen abruptly, include:
Body tremors
Diaphoresis (excessive sweating)
Tachycardia (rapid heart rate)
Hypertension
Fever
Delirium
Severe anxiety or agitation
Disorientation, hallucinations and seizures
Finding Detox and Treatment
There are many ways to get sober and no one "right" path. The first step is finding a reputable alcohol or other drug addiction treatment provider. You'll want to find a rehab center that has medically-supervised detox capabilities so that you can comfortably and safely detox from alcohol. There are inpatient and outpatient options, but an addiction specialist should determine the best level of care for you based on your individual needs. Effective addiction treatment providers will have addiction counselors, but they should also have mental health services as many people with alcoholism have co-occurring mental health conditions.
Strategies for Dealing with Alcohol Use Disorder: What to Say and Do
Attempting to help a loved one or friend who is struggling with an alcohol use disorder can be an emotional roller coaster. When an alcoholic is in active addiction, they can be defensive. Don't confront the behaviors while they're intoxicated. Find a time when they're sober and talk honestly about your concerns. Practice what you're going to say. Don't guilt-trip or assign blame; this is a disease. Offer support and use statements starting with "I" such as:
I see ...
I fear ...
I hope and expect ...
I will ...
I’m concerned about you because ...
Take action. Find support for yourself and other family members, too. Go to an Al-Anon or Alateen meeting or set up an appointment with a mental health professional. Learn to set healthy boundaries for yourself. At the end of the day, the person with addiction has to be willing to accept help.
SOURCE HAZELDEN BETTY FORD
We want to know your needs exactly so that we can provide the right solution for your loved one. Let us know what you want and we’ll do our best to help.
Copyright © All Rights Reserved.